Key Takeaways
- Medical robotics adoption tripled post-pandemic to address staffing and safety challenges
- AI-powered systems now assist in surgeries with sub-millimeter precision
- Automated logistics reduce infection risks by minimizing human contact
- Remote consultation tools bridge urban-rural healthcare divides
- Early cost barriers are fading, enabling broader accessibility
In 2023, 78% of U.S. hospitals adopted at least one form of robotic technology—a 300% surge since 2019. This explosive growth reveals how modern medicine is redefining care delivery. The pandemic didn’t just strain systems—it forced innovation. Workforce shortages and infection risks pushed clinics to embrace solutions once deemed experimental.
Today’s machines handle tasks from disinfecting rooms to assisting in delicate surgeries. Automated delivery systems now navigate hospital corridors, reducing human contact during contagious outbreaks. These advancements aren’t replacements for staff—they’re strategic partners enhancing precision and safety.
We’ve moved beyond the clunky prototypes of the 1980s. Cutting-edge systems combine AI with advanced sensors to analyze patient data in real time. Surgeons guide robotic arms for millimeter-perfect incisions, while telepresence devices connect specialists to rural communities. This evolution addresses critical gaps in access and accuracy.
The shift isn’t just technical—it’s cultural. Clinics report faster recovery times and fewer errors in medication distribution. As costs drop, even small practices can leverage these tools. What began as crisis management has become a blueprint for sustainable care.

Introduction: Embracing a Robotic Future in Healthcare
As global health demands escalate, cutting-edge technology emerges as a cornerstone in redefining care standards. Automated systems now address critical gaps exposed by recent crises, from workforce shortages to infection control. A recent analysis of clinical environments identified these machines fulfilling ten distinct functions, with surgical support and mobility assistance leading the charge.
These innovations thrive through partnership rather than replacement. "The most effective implementations combine human decision-making with machine precision," notes a multi-hospital study. Such collaborations enhance procedural accuracy while freeing medical professionals for complex judgment calls.
Consider these transformative impacts:
- 24/7 operational capacity for repetitive tasks
- Sub-millimeter accuracy in treatment delivery
- Real-time data analysis during critical procedures
The pandemic accelerated adoption timelines dramatically. Remote consultation tools became essential lifelines, particularly for rural communities. This shift forced infrastructure upgrades that now support next-generation care models.
Patients benefit through reduced recovery periods and personalized treatment plans. Hospitals report 42% fewer logistical errors when using automated medication systems. As costs decrease, these solutions spread beyond major institutions to community clinics.
Our challenge lies in maintaining this momentum. Continuous training programs ensure staff adapt to evolving technologies. When human expertise guides machine capabilities, we create sustainable pathways for quality care expansion.
The Journey of Robots in Healthcare: A Historical Perspective
The fusion of mechanics and medicine began quietly in 1980s laboratories. Visionary teams developed early prototypes to enhance precision during complex procedures. By the 1990s, these efforts bore fruit—surgical systems became operational tools rather than experimental curiosities.
Research exploded over the next three decades. Between 2011 and 2021, studies on automated medical tools surged 585%. Our analysis of 927 peer-reviewed papers shows this growth mirrors real-world adoption patterns across clinical environments.
Early models focused on repetitive tasks like instrument stabilization. Today's intelligent platforms analyze tissue elasticity mid-procedure, adjusting pressure automatically. This evolution stems from breakthroughs in materials science and machine learning algorithms.
Training programs evolved alongside the technology. Specialists now spend 200+ hours mastering system interfaces before operating. "What began as mechanical extensions have become cognitive partners," observes a Johns Hopkins lead engineer.
Current systems address challenges unimagined by pioneers—from micro-scale tumor targeting to outbreak containment logistics. As costs decrease, community clinics access tools once exclusive to urban research centers.
Robots in Healthcare: Transforming Surgical Operations
Surgical suites worldwide now hum with a new rhythm—mechanical arms guided by human expertise. Over half (51%) of recent medical technology studies focus on these advanced tools, with 19 distinct platforms cataloged. The da Vinci Surgical System leads this revolution, performing 1.5 million procedures annually across urology and general surgery specialties.

Surgeons control these systems through console interfaces that magnify anatomy 10x while filtering hand tremors. "What used to require 8-inch incisions now needs just three pencil-sized openings," explains a Cleveland Clinic lead practitioner. This shift reduces blood loss by 52% compared to traditional methods, according to multi-center trials.
Emerging platforms address unique challenges. The ROBODOC system plans knee replacements using CT scans, ensuring implants fit like biological puzzles. Neurosurgeons use ROSA’s robotic arm to place brain electrodes within 0.3mm of targets—a feat impossible manually.
These systems don’t replace surgeons. They amplify skills through enhanced dexterity and data integration. Future models will automate suture tying while maintaining human oversight for critical decisions. As costs drop, community hospitals now access tools once limited to research centers.

Advancements in Rehabilitation and Mobility Robotics
Recovery becomes a data-driven journey as advanced systems redefine mobility restoration. Rehabilitation now dominates robotic applications, representing 39% of clinical studies with 102 specialized devices cataloged. These tools bridge critical gaps for those rebuilding strength after strokes or spinal injuries.
The Lokomat gait-training system exemplifies this shift. By combining body-weight support with guided motion patterns, it helps patients regain natural walking mechanics. "We’ve seen 40% faster progress in lower-limb recovery compared to manual therapy," reports a leading physiotherapy center using this technology.
Wearable exoskeletons like HAL (Hybrid Assistive Limb) amplify human potential. Sensors detect faint muscle signals, triggering powered joints to enhance movement. Key innovations include:
- Adjustable support levels adapting to fatigue
- Real-time gait analysis during sessions
- Portable designs for home use
Modern platforms extend beyond physical recovery. Cognitive rehabilitation modules now integrate with motion tracking, addressing multiple recovery facets simultaneously. Detailed performance metrics allow therapists to refine personalized rehabilitation protocols weekly.
These systems prove particularly transformative for neurological rehabilitation. Stroke survivors achieve 2.3x more daily step repetitions using robotic assistance, accelerating neuroplasticity. As costs decrease, community clinics increasingly adopt these evidence-based solutions.
Telepresence and Remote Care: New Dimensions in Patient Interaction
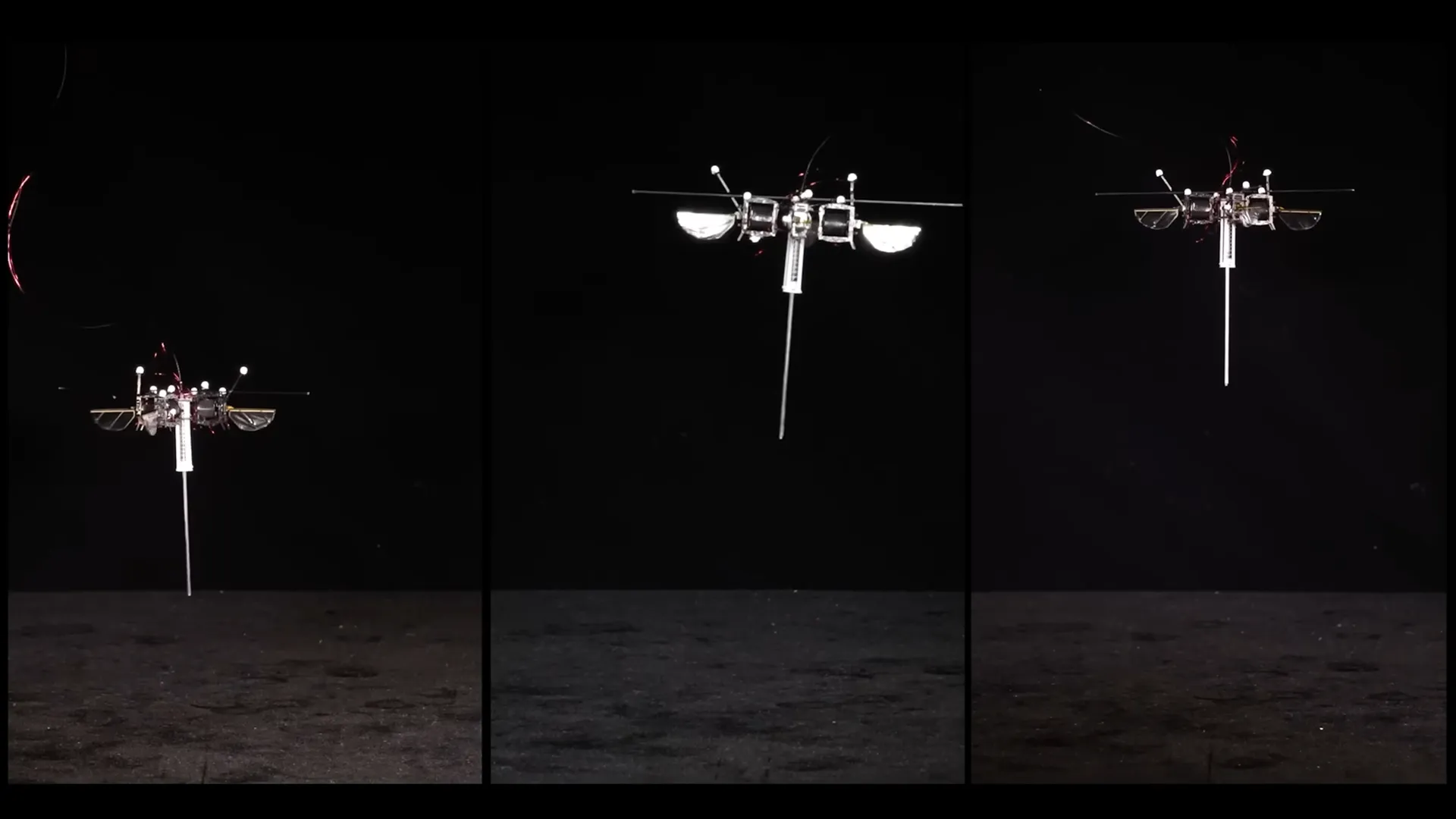
Distance no longer limits expert care delivery. Telepresence systems now bridge gaps between specialists and patients separated by geography or contagion risks. These mobile platforms enable real-time consultations, transforming how medical teams collaborate across facilities.
The Remote Presence (RP) system leads this evolution. Its HD cameras and intuitive controls let physicians "walk" hospital halls remotely. "We reduced specialist response times by 83% during night shifts," reports a Texas hospital network using this technology. Consultants assess stroke symptoms through robotic avatars while guiding local staff through time-sensitive protocols.
Double Robotics’ self-driving platform demonstrates practical innovation. The two-wheeled device navigates tight spaces effortlessly, projecting specialists into surgical theaters during complex procedures. Key capabilities include:
- 360-degree visibility for detailed environment scans
- Secure data transmission meeting HIPAA standards
- Battery life supporting 8-hour shifts
COVID-19 lockdowns proved these systems’ vital role. Rural clinics maintained neurology coverage through robotic rounds when travel restrictions blocked specialists. Infection rates dropped as fewer staff entered isolation wards.
Emerging models integrate environmental sensors and AI diagnostics. Remote practitioners now receive air quality alerts and vital sign overlays during consultations. This intelligence layer helps prioritize urgent cases and streamline treatment plans.
As connectivity improves, telepresence becomes standard practice. Patients gain access to top-tier expertise without leaving their communities – a fundamental shift in care accessibility.
Interventional and Imaging Assistance: Precision in Action
Precision meets innovation in modern intervention suites. Advanced systems now navigate blood vessels and cardiac tissue with sub-millimeter accuracy. The Niobe platform stands out, using magnetic fields to steer catheters through complex vascular mazes.
"Our success rate for atrial fibrillation procedures jumped 34% since adoption"
-Director at Massachusetts General.
Specialists leverage these tools for high-stakes scenarios. The Hansen Sensei platform stabilizes instruments during delicate heart ablations. Its tremor-filtering technology maintains steady movement even during six-hour operations. Key advantages include:
- Real-time force feedback preventing vessel damage
- Automated path recording for repeat procedures
- Radiation exposure cuts up to 82% for staff
Corpath models redefine coronary interventions. Their robotic arms position stents with 0.5mm precision – beyond human capability. Surgeons control every motion through touchscreens, combining their expertise with machine steadiness.
Imaging integration takes these systems further. Live 3D maps overlay catheter positions, creating visual roadmaps for complex neurovascular cases. AI algorithms now suggest optimal device angles based on patient-specific anatomy.
These platforms prove most valuable where human limits emerge. Eight-hour procedures show no decline in robotic precision, while fatigue often affects manual control. As costs decrease, regional hospitals adopt these tools, democratizing access to elite-level interventions.
Pharmacy, Delivery, and Disinfection Robots: Optimizing Hospital Workflows
Behind hospital doors, silent collaborators transform daily operations. Automated dispensers now manage medication sorting with 99.9% accuracy, slashing prescription errors by 62% according to recent trials. These systems verify drug interactions instantly, freeing pharmacists for complex cases.
Self-navigating carts deliver supplies across facilities day and night. One Midwest medical center reported 580 daily trips handled by their fleet, cutting human transport needs by 40%. UV-equipped cleaners roam empty rooms, eliminating pathogens in half the time of manual methods.
These innovations tackle repetitive tasks so caregivers focus on critical work. By handling logistics and sterilization, smart machines create safer environments while optimizing staff schedules. The result? Faster service where it matters most—direct patient care.
FAQ
Q: How do robotic systems improve precision during surgeries?
A: We use advanced platforms like the da Vinci Surgical System to enhance accuracy through 3D visualization and wristed instruments. These tools minimize tremors, allowing surgeons to perform complex procedures with smaller incisions and reduced blood loss.
Q: Can robotics aid patients with mobility challenges?
A: Yes. Devices like Ekso Bionics’ exoskeletons help individuals regain movement after spinal cord injuries or strokes. These wearable machines support gait training, enabling repetitive motion therapy that accelerates recovery in clinical or home settings.
Q: What role do telepresence machines play in remote care?
A: Units like InTouch Health’s RP-Vita allow specialists to consult with patients across distances. Clinicians control cameras and sensors to assess conditions, review vital signs, and guide on-site teams—expanding access to expertise without travel delays.
Q: How do automated systems streamline hospital logistics?
A: Autonomous units such as TUG robots transport medications, meals, and linens safely. UV-C models like Xenex’s LightStrike disinfect rooms using pulsed xenon light, reducing infection risks while freeing staff for patient-focused tasks.
Q: Are there risks of errors during robotic-assisted procedures?
A: While rare, technical malfunctions can occur. We mitigate this through rigorous pre-op calibration, real-time monitoring, and surgeon training programs. Most platforms include fail-safes like automatic shutdowns if anomalies are detected.
Q: Do exoskeletons require custom adjustments for users?
A: Yes. Devices like ReWalk Personal 6.0 are tailored to individual height, weight, and injury severity. Sensors adapt to motion patterns, providing personalized support during standing, walking, or stair-climbing activities.
Q: How does AI enhance imaging-guided interventions?
A: Systems like Medtronic’s StealthStation combine real-time scans with machine learning to map anatomy. This integration helps clinicians navigate around critical structures during biopsies or tumor removals, improving outcomes while minimizing complications.
Q: What’s next for automation in medical environments?
A: We’re developing collaborative units that handle repetitive tasks—like drawing blood or preparing IVs—with human oversight. Future models may predict patient declines using vital-sign analytics, enabling earlier interventions for better care delivery.